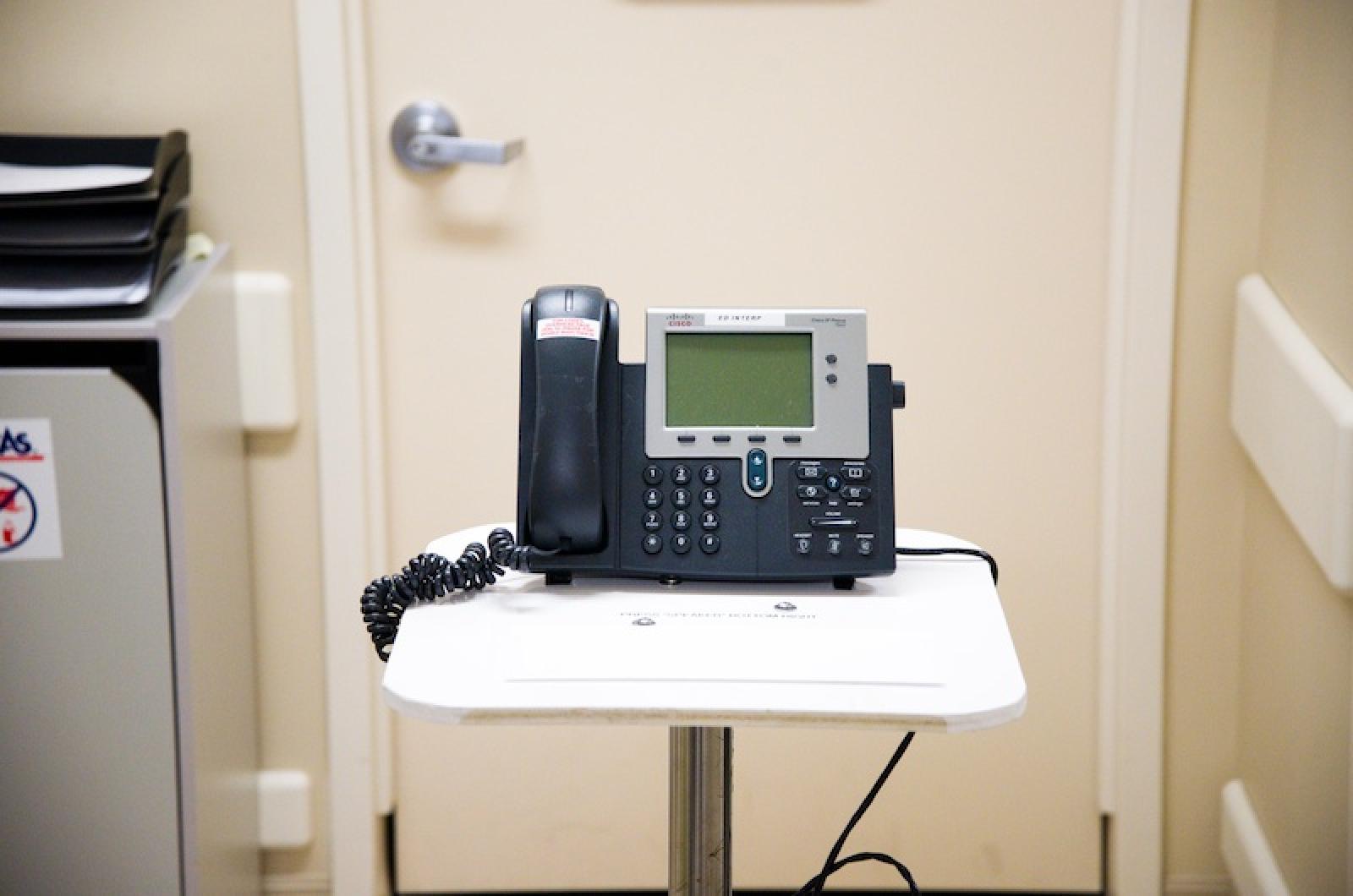
One year after a program using a live interpreter was discontinued at the Martha’s Vineyard Hospital, patients and medical providers say the replacement system, which uses an electronic telephone program instead of a person, is meeting needs adequately — if not as personably.
Twelve months ago this week the hospital replaced its interpreter program with an AT&T telephone interpreter service. The decision was purely a cost-saving measure; the hospital had suffered its first operating loss in a decade, and the interpreter program was costing about $100,000 a year.
“We needed to cut costs,” said Deedee Wheeler, chief quality and corporate compliance officer at the hospital. “If I have to cut . . . I want it not to affect quality in any way.”

Last year, about five per cent of hospital patients required the services of an interpreter. The hospital has spent less than $20,000 on the telephone interpreter service since ending a contract that allowed for live interpreters in the emergency room and throughout the hospital. The mission of the hospital is to provide and arrange for high-quality, accessible medical care to anyone who needs care, regardless of the ability to pay.
The interpreter program was started in 2006 to address the health care needs of the Brazilian community. Planning grants allowed the Island Health Plan, an independent nonprofit that operates a walk-in clinic in Edgartown, to develop and launch the program by training more than 20 interpreters. The hospital paid employees of Island Health Plan for their interpreter services.
“They were sad to see it go but felt that it had to happen,” said Cynthia Mitchell, director of the Island Health Plan. “The hospital effectively eliminated our ability to keep it running.”
“We gave notice,” said Timothy Walsh, president and chief executive officer of the hospital, in an email. “We had just finished our fiscal year where we lost $600,000.”
Along with savings gleaned, switching to the telephone service has improved response time in the emergency room, where the hospital fields about half of its interpreting needs.
“It could be 20 to 30 minutes for an interpreter to get there,” said Dr. Jeffrey Zack, director of the emergency room, in an interview this week. “In some ways it’s sort of enhanced. We get to the bottom of what’s going on in a matter of minutes. In an emergency that can make a difference.”

Under the old program, a team of interpreters trained and worked together. A few interpreters spoke Spanish and French but the majority of the demand was for Brazilian Portuguese. They wore beepers and showed up at the hospital when their services were needed. Typically interpreters worked a minimum shift of two hours, Mrs. Wheeler said.
“We used them all the time,” said Daisy Pattison, a longtime registered nurse at the hospital. “It was a really fabulous service.”
Critics of the switch say the telephone conversations don’t convey facial expressions and other types of nonverbal language, and they also say that given the years of effort and grant money spent creating the program, cutting it seemed wasteful. Some said they thought the funds could have been managed more effectively, but the problem for the hospital is that it provides full-service health care all year long, which means sometimes a team of professionals are on the clock even when the emergency room may be empty.
“After the end of the medical interpreter program, those in the Brazilian community who do not speak English are finding it more difficult to receive appropriate health care,” said Maria Mouzinho, the community outreach health educator at the Vineyard Health Care Access Program, in an email to the Gazette. Her job involves speaking with clients about eligibility for various health programs.
“Since they are not able to communicate, they depend on others, maybe a family member who could be a child, to go with them to their doctor visits, going to the lab, physical, therapy, etc,” she wrote.
Since eliminating the personal interpreter program, the hospital has spent less than $20,000 on the telephone service. But some of the interpreters still get work now from patients who pay them for their services. Many who prefer in-person interpretation bring family members or pay interpreters on their own.
“You can be an advocate for the patient,” said Dilcelia Guimarães, who trained in the program, translated at the hospital and now works at Island Health Clinic in Edgartown. “Most patients understand, they’re just afraid to speak.”
Liz DiCarlo, project coordinator for the Lighthouse Alliance Grant, a group devoted to making health care accessible, echoed the sentiment.
“People need to have their care delivered in a culturally competent way,” she said.





Comments (1)
Comments
Comment policy »