A broad-based effort to combat Lyme disease is now underway on the Vineyard, with the objective of better documenting and preventing the tick-borne illness that has affected untold numbers of year-round Islanders, summer residents and casual visitors.
For the past two weeks a team of medical, nursing and pharmacy students from the University of Massachusetts have descended on Island ferries, churches and pharmacies to interview health officials and vulnerable populations about their relationship to a disease that has been notoriously difficult to assess and manage effectively. The student team will present their findings at a public session this afternoon at 4:15 p.m. at the Martha’s Vineyard Regional High School cafeteria.
It’s all part of $250,000 five-year study aimed at reducing the incidence and severity of Lyme disease on the Vineyard.
“It’s a now-or-never kind of thing,” said Edgartown health agent Matt Poole, who is involved in the study.
Led by the Island boards of health, the study is nearing the end of its first year. Funding for the study comes from a state-mandated grant through the Martha’s Vineyard Hospital known as a community health initiative. The grant will provide $51,670 each year for five years to the boards of health.
So far that money has been earmarked for a variety of projects, including blood tests and yard assessments on Chappaquiddick and Naushon islands, a tick-borne illness-related curriculum for Island students, the development of streamlined reporting systems for health care providers, and the survey and interview work of the University of Massachusetts students. This winter Mr. Poole said the towns will also contract with a firm to perform aerial transects of Chappaquiddick, using thermal imaging to determine the size of the deer population.
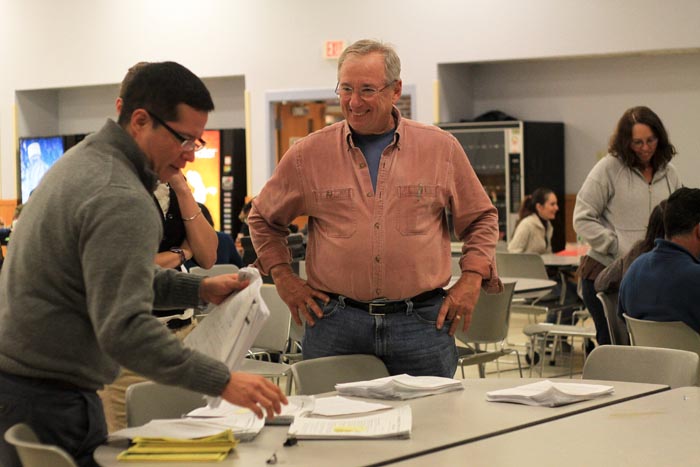
On Wednesday night this week, second-year University of Massachusetts medical students Sebastian Ramos and Sara Weiner dropped in on an English-as-a-second-language night class at the high school.
“Tem cuidado!” Mr. Ramos relayed through translator Vera Cacique when one student inquired about the risks of infection during hunting.
When the students were asked whether they knew anyone who had Lyme disease, three-quarters of the room raised hands.
Mr. Poole is not surprised. He said the officially-reported Lyme disease cases do not reflect the actual incidence of the disease here. According to the Centers for Disease Control, in 2010 there were 25 reported cases of Lyme disease in Dukes County.
“All of the numbers are suspect at this point,” Mr. Poole said. “The CDC says there are 30 confirmed cases of Lyme on Martha’s Vineyard. If you think long and hard enough, you could probably come up with more than 30. Our goal is to have a higher level of confidence in the data.”
The small island of Chappaquiddick has been a laboratory of sorts for the work of the study group. In August Mr. Poole, along with Tufts infectious diseases professor Sam Telford, Island biologist Dick Johnson and nurses from the Vineyard Nursing Association set up a makeshift blood sampling depot at the Chappy fire station. A total of 30 residents, nearly a fifth of the year-round population, volunteered to participate in the blood sampling and survey work. The results of those tests are not yet available.
“Chappaquiddick is an ideal place to study because it’s a geographically-isolated population,” Mr. Poole said. While on Chappaquiddick, Mr. Telford also performed sweeps of residential properties with cheesecloth to assess the number of deer ticks present in the environment. Mr. Poole said reducing tick habitat by clearing out leaf litter and reducing shade can go a long way toward reducing a homeowner’s exposure to the disease.
To Tisbury board of health member Michael Loberg, establishing a baseline of data is a prerequisite before the boards can issue any Islandwide recommendations, but he said the preventative value of public education cannot be underestimated. This week the boards of health went live with a Web site (mvboh.org) designed to serve as a centralized source of information on Lyme disease and other regional health issues.
“We think there are tremendous opportunities in improving education,” said Mr. Loberg. To that end, the boards of health have also established a newfound presence in the schools, having already visited Island elementary school health classes with plans to do the same at the high school in the coming year.
“The idea is to do this tick education curriculum on an ongoing basis so that the kids will take it home to their parents, that’s the best way to get it into the household,” he said.
By the end of next year Mr. Loberg said the boards of health will be ready to make their recommendations to the all-Island selectmen about how to reduce the incidence and severity of the disease, but he said it was too early to speculate on what form those may take. When they were planning the grant application, health agents had discussed the idea of making venison more widely available through the Island Grown Initiative as a way of promoting hunting.
“Increased hunting could be a recommendation, but only if there’s data that reducing the deer population has an effect,” said Mr. Loberg. “We will follow the data so we’ll have to see.”
He said the boards of health may eventually apply for funding through the Centers for Disease Control or the National Institutes of Health to put into effect a plan of action in the coming years.
Yesterday the university medical team was still compiling data in their temporary New York avenue house, entering the 1,000 some-odd surveys gathered during the previous two weeks and sifting through the data in preparation for their presentation at the high school. Some of the students are rural health scholars, on-Island to study the unique challenges endemic to sparsely populated or isolated communities. For second-year medical student Sebastian Ramos, it has been an experience he hopes to bring back to his native Guatemala.
“I grew up in a very rural area, 2,000 people at most, so my first experience with physicians was that’s the guy who came over when you were sick,” he said. “I never saw the inside of a clinic or anything until I was in the States. The opportunity to be here in this community has been wonderful — I guess that’s part of the project, to be in a rural area and really feel like you’re part of the community. We’ve only been here for two weeks but the community — from the people on the ferry, to the [Wampanoag] tribe, to the Brazilian community have really made us feel welcome.”
The night before, second-year medical student Daniel Wemple and second-year graduate nursing student Meghan King visited a Brazilian church where grocer Elio Silva translated for the congregation.
“They took the survey very seriously,” said Ms. King.
“We got a great response,” said Mr. Wemple. “People really seemed hungry for more information.”







Comments
Comment policy »